By Lauren Schaffer
Note: Essay 4 in a series, all from Dr. Amanda McVety’s Spring 2019 class on Medicine and Disease in Modern Society
The air is warm and muggy. A faint buzzing echoes in the air, and neck hairs tingle. The acrid smell of smoke fills nostrils, as bark nests are burned in an attempt to ward off an impending illness: malaria. This is what people may have experienced in 1930s southeast America, where the disease devastated many towns near the waters where mosquitos flourished.Biologically, the disease was understood to be a cycle of chills and fevers, a parasitic infection caused by the bite of an Anopheles mosquito or the drinking of infected waters where they resided and bred. Socially, many people lived in fear because it was difficult to be sure whether or not a given mosquito or water source was infectious. There was not a classist or isolationist attitude associated with malaria, but there was a geographic or regional predisposition surrounding who contracted the disease.
Between 1930 and 1940, the majority of what people knew about malaria came from abroad, because that was where the disease originated and primarily attacked. Africa, India, and south Asia were common places to contract malaria, and people were infected in droves, resulting in hundreds of thousands of deaths.[1] When it first reached America, the government questioned whether or not there should be a quarantine because they were unsure of its contagion capabilities.[2] Soon, doctors and citizens alike knew how the disease was spread, through the various discharges of the Anopheles mosquito, but it was difficult for the average person to differentiate between it and the common American Culex variety. Its body is much narrower and sharper, and only this species carries the parasites that cause infection.[3] People who drank water from sources where these insects mated were also at risk of contracting the disease, because the parasites can be secreted into the water during mating.
Once bitten, a victim begins to feel chills, which the body responds to with feverishness. This sequence repeats, and often induces nausea, vomiting, and jaundice, or yellowing of the skin. The main reason people die from malaria is due to these excessive lapses outside homeostasis, which is exhaustive and cannot be maintained, as it wears out the immune system.[4] Primarily, 20th century doctors would prescribe people to bed rest for 10-15 days, which is usually how long it took to recover if survivable. Many victims, however, could face up to five years of relapse, and at the time they had no reason as to why this occurred in some cases and not others.[5] The peak mortality rate of malaria in America was 3.3 deaths per 100,000 persons, in 1933.[6] Though the death rate was not massive, it was higher than typical, and this fact combined with the imminent reality of often being outside terrified the public.
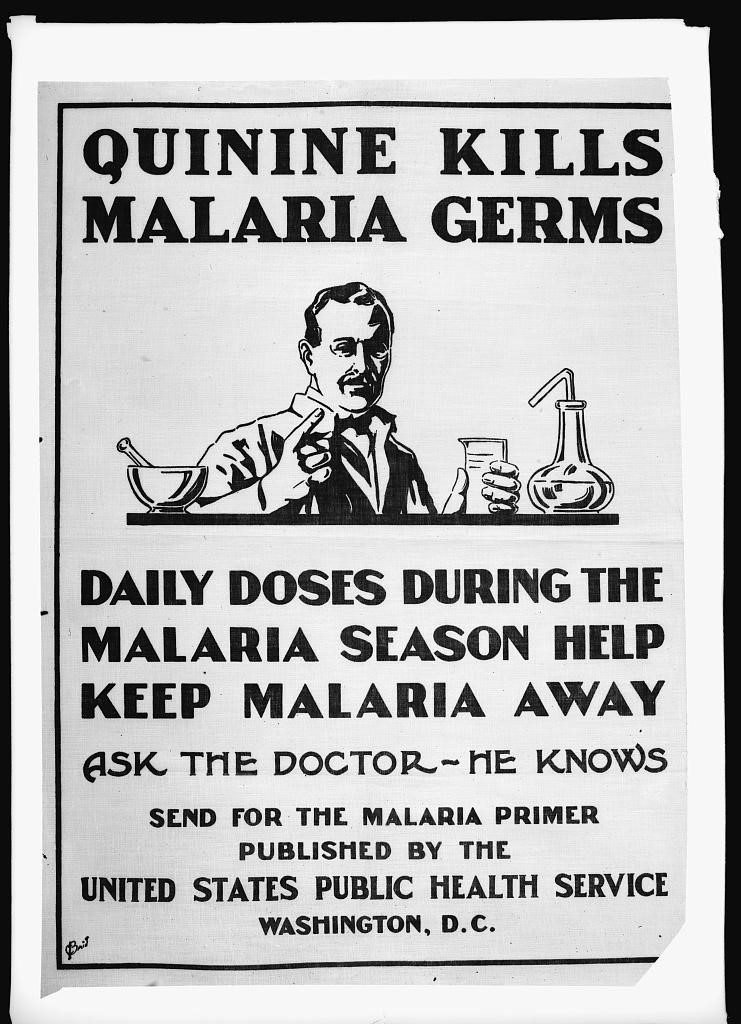
The fact that there was no real cure did not help curb this paranoia. Treatment for malaria was fairly limited to taking quinine, a substance extracted from the bark of cinchona trees, which is also found in tonic water. It was first discovered in South America in 1820, when bark was a main source of medicinal products for varying diseases.[7] At this time, it was recommended in encapsulated pills, since it absorbed better that way versus through an injection. The recommended dosage was 30 grains per day to break chills, then 10 grains daily at bedtime to break the attack, though relapse was still possible.[8] Plasmochin was also effective for killing the parasite, but not to alleviate symptoms. It was not advised to take quinine daily to prevent, only once the disease had been contracted. Throughout the history of malaria, drugs like quinine were often abused, and used as a vaccine instead of a symptomatic relief.[9]
In order to prevent malaria before it began, many infrastructural precautions were taken in areas of the southeast, such as Tennessee, Mississippi, and Alabama, where it was most prevalent. Water reservoirs were seized by health departments and inspected, and persons living within a two-mile radius were tested regularly. Special bureaus were commissioned explicitly for the investigation and prevention of malaria, specifically by the TVA in Tennessee.[10] Mosquito nets covered many people as they went outside, and were also placed over food and other high-risk items. This became and issue, however, because the majority of malaria casualties stemmed from children, those with outdoor professions, and persons living and working in rural areas. These water treatments and net coverings did not bode well for working in such sparse areas where being among the marshes and cotton fields was their livelihood. One solution proposed at the time was to grow legume plants, such as beans and alfalfa, as it had been observed in other countries that crops such as these somehow fended off the mosquitoes.[11]
Now, scientists know about many different factors that contribute to who gets malaria, why, and how to prevent it. There are several antibiotics in place that can treat it, quinine still being one of them. Other drugs including chloroquine, doxycycline, mefloquine, and more are used to treat the disease as well, sometimes in conjunction with quinine.[12] Much of this is dependent on the type of parasite the mosquito hosts and infects the person with, as well as other illness they may have, allergies, area of contraction, etc. In addition, a much wider spread of insecticides and bug zappers are available to protect people day-to-day from these potentially deadly insects. Doctors are also aware of certain genes people hailing from Africa and parts of the Middle East carry, which mutates their blood cells in a way that immunizes them from malaria (such as sickle cell disease).[13]
Altogether, malaria is and was a lasting, horrific disease that still affects millions of people today. Even though scientists know much more about it at a molecular, chemical, and human level, it still kills and is being investigated further. No permanent treatment or vaccine exists yet, and many children and adults even now suffer immensely, especially in underfunded and underdeveloped countries. By looking at how people experienced the disease earlier in history, researchers can compare the information they have now and perhaps learn from both their mistakes and advancements, in order to try and eradicate the menace that is malaria.
Bibliography
Copeland, Royal S., M.D. “Guarding Your Health: Control of Malaria.” The Cincinnati Enquirer, June 27, 1931. Accessed March 1, 2019. https://search.proquest.com/docview/1882058259/1067A9A0CC8E46C4PQ/5?accountid=12434.
Evans, Dr. W. A., M.D. “How To Keep Well: Treatment for Control of Malaria.” The Washington Post (Washington, D.C.), October 29, 1932. Accessed February 28, 2019. https://search.proquest.com/hnpwashingtonpost/docview/150244363/6D227B296E294483PQ/3?accountid=12434.
Krysto, Theo. “Can the World Banish Malaria?” Scientific American, 142 (April 1930): 270-72. Accessed February 28, 2019. https://web.b.ebscohost.com/ehost/detail/detail?vid=0&sid=9c050e8e-219b-490f-a767-6a23adca6093%40pdc-v-sessmgr05&bdata=JnNpdGU9ZWhvc3QtbGl2ZSZzY29wZT1zaXRl#AN=514363711&db=rgr
Malar, J. “Quinine, an old anti-malarial drug in a modern world: role in the treatment of malaria” US National Library of Medicine, May 24, 2011. Accessed April 19, 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121651/
“Malaria: MedlinePlus Medical Encyclopedia.” MedlinePlus. January 28, 2019. Accessed March 01, 2019. https://medlineplus.gov/ency/article/000621.htm.
“Mighty Malaria.” Time Magazine, January 14, 1935. Accessed March 1, 2019. https://web.b.ebscohost.com/ehost/detail/detail?vid=11&sid=51785a60-de75-41e4-b5cf-c234fa1fdf0a@pdc-v-sessmgr01&bdata=JnNpdGU9ZWhvc3QtbGl2ZSZzY29wZT1zaXRl#AN=54805106&db=a9h.
Porter, Russell B. “Malaria Scourge Fought By the TVA.” The New York Times, April 24, 1938. https://search.proquest.com/docview/102570606/abstract/7097FAF45CDB4552PQ/1?accountid=12434.
Snowden, Frank M. The Global Challenge of Malaria: Past Lessons and Future Prospects. New Jersey: World Scientific, 2014.
U.S. Congress. Senate. Committee on Public Health and National Quarantine. Malaria and Typhoid Fever: Hearings before the United States Senate Committee on Public Health and National Quarantine, Sixty-Third Congress, Second Session, on Mar. 5, 6, 1914. 63rd Cong., 2d sess. S. Bill. Washington: U.S. G.P.O., 1914.
U.S. Public Health Service.
American Red Cross. “Quinine kills malaria germs” Library of Congress, September 9, 1920. https://www.loc.gov/item/2017677870/
[1] Frank Snowden, The Global Challenge of Malaria: Past Lessons and Future Prospects (New Jersey: World Scientific, 2014), 29-30
[2] US Congress, Malaria and Typhoid Fever: Hearings before the United States Senate Committee on Public Health and National Quarantine (Washington, U.S., 1914)
[3] Theo Krysto, Can the World Banish Malaria? (Scientific American, 1930), 270-272
[4] MedlinePlus, Malaria: MedlinePlus Medical Encyclopedia (MedlinePlus, 2019)
[5] Royal Copeland, Guarding Your Health: Control of Malaria (The Cincinnati Enquirer, 1931)
[6] Snowden, 2014, 78
[7] J. Malar, Quinine, an old anti-malarial drug in a modern world: role in the treatment of malaria (US National Library of Medicine, 2011)
[8] Mighty Malaria (Time Magazine, 1935)
[9] W. A. Evans, How to Keep Well: Treatment for Control of Malaria (The Washington Post, 1932)
[10] Russell Porter, Malaria Scourge Fought by the TVA (The New York Times, 1938)
[11] Theo Krysto, 1930
[12] MedlinePlus, 2019
[13]Snowden, 2014,142-145


